Vladimir Garcia Lozada explores the use of zygomatic implants, an efficient and predictable therapeutic option for rehabilitation of patients with severe maxillary bone resorptions.
The use of zygomatic implants for the rehabilitation of the atrophic maxilla using the Bränemark protocol was first developed in 1998. The journey in the more than 20 years since has seen a huge number of advancements.
These implants have proven to be an efficient and predictable therapeutic option for rehabilitation of patients with severe maxillary bone resorptions, demonstrating high success rates according to various studies.
They offer multiple advantages for patients suffering maxillary atrophy, enabling rehabilitation while reducing treatment time and morbidity associated with extensive or large reconstructive bone grafts procedures, restoring function and aesthetics, and marked improvement in quality of life.
This treatment modality has undergone various surgical approaches, refined to enhance protocol efficiency and prevent complications, thereby optimising success rates. Critical anatomical, biological, biomechanical, and biofunctional factors inherent to this procedure are carefully considered (Garcia-Lozada, 2023).
Zygomatic implants: techniques and approaches
In the late 1990s, the classic Bränemark zygomatic implant technique involved a single implant placement in each zygomatic bone (one bilaterally) positioned very palatally, and splinted alongside to two to four conventional implants in the premaxilla (anterior region).
In 2003, Bothur and Balshi published articles on the ‘use of multiple zygomatic implants’ for patients without adequate anterior and posterior maxillary bone, paving the way for research and development of complete maxillary bone insufficiency cases, including both anterior and posterior maxilla regions.
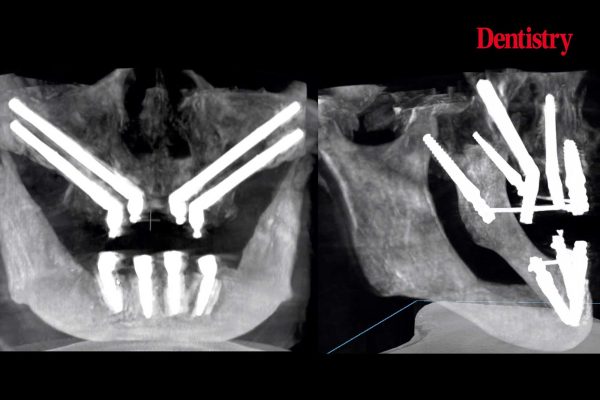
The quadzygoma or zygoma quadruple approach (quad zygomatic implants), involving four zygomatic implants placement, where two zygomatic implants are placed bilaterally in each zygomatic bone and then splinted, provided an effective solution for patients presenting complete maxillary bone insufficiency, as well as the unilateral approach that use a single zygomatic implant in one zygomatic bone splinted to conventional implants (Garcia-Lozada, 2018).
From the initial Bränemark protocol in 1998, new approaches emerged to improve and optimise the technique, including:
- Slot technique (Stella and Warner, 2000)
- Exteriorised approach (Migliorança, 2006)
- Extrasinus approach (Aparicio, 2006)
- Extramaxillary approach (Maló, 2008)
- Extrasinusal path (Chow, 2010).
Despite these contributions, a clear consensus on selecting the optimal approach for each case was lacking until 2011, when Aparicio published the ZAGA classification (zygomatic anatomy-guided approach). This holistic anatomy-based classification, as well as prosthetic requirements, established guidelines for zygomatic implant trajectory placement optimisation and became a global reference consensus, further solidified in 2012 with the textbook Zygomatic Implants – The Anatomy-Guided Approach (ZAGA).
Planning and tools
Digital technologies play an essential role in zygomatic implant surgery planning and execution. These include panoramic radiographs, TC scanners and CBCT, virtual planning software, 3D-printed stereolithographic models, static bone-supported guides, modular or stackable guides for immediate-loading prosthesis, dynamic intraoperative navigation systems like a GPS (real-time tracking) and robotic implant surgery.
We will certainly be seeing more artificial intelligence (AI) tools in the near future. However, operator experience and skills remain crucial to perform this sensitive and more complex surgical technique.
Teeth in a day
Immediate loading concept or ‘teeth in a day’ on zygomatic implants has proven a highly effective protocol, supported by extensive studies. Bedrossian and Chow pioneered this approach in 2006, followed by Duarte (2007) as well as Davó and Kuabara (2010).
For both cases, a classical approach was used with two ZIs splinted with conventional implants and quad zygomatic implants with four zygomatic implants splinted, enabling patients to acquire fixed provisional prosthesis the same day of zygomatic implants surgery, reducing treatment time and recovering function, aesthetics with quality-of-life improvement.
Biomechanics in zygomatic implant procedures is related to an optimal implant distribution on the maxillary arch as well as the correct prosthesis passive fit and distribution of the occlusal forces and loads.
Depending on the case, additional support can be achieved with conventional implant placements in the anterior region (premaxilla) or in the posterior region with tuberosity-pterygoid implants, enhancing the anterior-posterior spread to minimise cantilevers. A rigid, screw-retained prosthesis with passive fit and balanced occlusion is critical for long-term success.
Zygomatic implant design
Another factor to take into consideration for the refinement of this technique is the implant design. Just as the evolution of approaches and techniques has been presented among many other factors to improve this protocol, the zygomatic implant designs have also evolved over the time in terms of their macrogeometry, treatment surface, and prosthetic connection.
Therefore, the zygomatic implants can be classified in terms of design into three zones: apical zone, intermediate zone and coronal zone. Depending on the zygomatic implant system used, we can use these zones to observe and find the greatest differences and similarities between the various existing systems.
It should be noted that depending on the particular case to be treated, there may be designs that favour better biological and functional behaviour, combined with the approach applied, the surgical prevention measures carried out and the adequate prosthetic execution (Garcia-Lozada, 2023).
Complications
Potential complications may include rhinosinusitis (linked to intrasinus trajectories) and vestibular dehiscence (associated with extramaxillary paths). Preventive measures to avoid these common complications involve knowledge and skills set, meticulous planning, incision design, zygomatic implant design selection, tissues preservation, zygomatic implants path or trajectory and adjunct techniques like pediculated connective tissue grafts, and buccal fat pad covering, among others.
Continuous refinement is guided by success criteria such as Aparicio’s zygomatic implants success criteria (2011), the ORIS success criteria (2020), and zygomatic implants Critical Zones (2021), alongside complication management protocols (Bedrossian, 2018).
Over my exciting journey using and teaching the zygomatic implant concept as a globally extended technique, contributing through publications, training and mentoring remains deeply motivating. Mastering the zygomatic implant technique demands rigorous, meticulous and continuous learning. Even more so for those who perform this protocol systematically with respect to the patients’ safety and their predictable rehabilitation, with the know-how in prevention and management of complications.
For references, email newsdesk@fmc.co.uk.
Save 40.0% on select products from L&L First Aid with promo code 40G4RTOE, through 4/11 while supplies last.
Source link