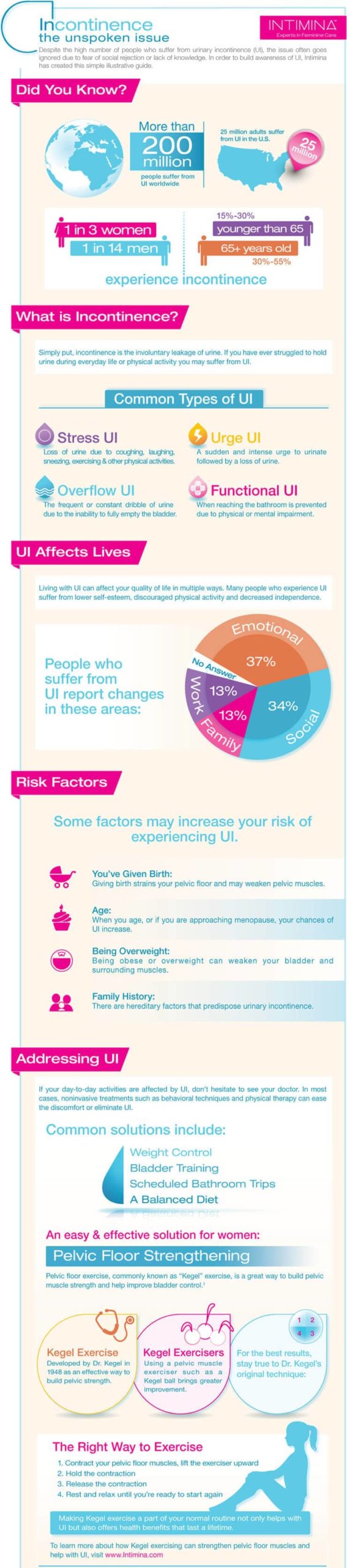
Urinary incontinence is an extremely common problem that affects more than 200 million people around the world. On average, one in three women and one in fourteen men will experience urinary incontinence at some point in their lives. 15-30% of sufferers are younger than 65 years old, and 30-55% of sufferers are over the age of 65.
Despite its prevalence, urinary incontinence still holds a shameful stigma for many people. Understanding how common this condition is, the risk factors behind it, and what you can do to address it is the first step towards destigmatizing such a common condition and reducing unnecessary discomfort and shame.
What Is Incontinence?
Urinary incontinence, or UI, refers to the loss of bladder control. The severity of this condition ranges widely, from a small leakage when you laugh or sneeze too hard to being totally unable to control when and where you urinate. There are several types of urinary incontinence that we’ve listed below in order of severity.
1. Stress incontinence
Urine occasionally leaks when sudden, heavy pressure is exerted on your bladder. This may happen when laughing extremely hard, coughing, performing certain exercises, or lifting a heavy object.
2. Urge incontinence
An intense, sudden urge to urinate, accompanied by an involuntary release of urine. You may urinate excessively, including during nighttime and when you sleep. This type of incontinence may be the result of a minor condition like a bladder infection or a more severe condition such as diabetes or a neurological problem.
3. Functional incontinence
A mental or physical impairment prevents you from being able to get to the toilet in time to relieve yourself. If you have severe arthritis, for example, you may not be able to get your pants off quickly enough.
4. Mixed incontinence
A combination of different types of urinary incontinence. The most common type of mixed incontinence is stress and urge incontinence.
5. Overflow incontinence
Your bladder doesn’t empty completely, causing you to experience frequent or constant dribbling of urine.
Although UI is more prevalent in aging populations, it isn’t something that every aging person experiences. If you think that UI is impacting the way you go about your life, it’s important to address the issue with your doctor as soon as possible. Often, basic dietary and lifestyle changes or simple medical intervention can alleviate these symptoms.
Risk Factors For Incontinence
Gender
Women are significantly more likely to have stress incontinence due to their anatomical makeup and life events like menopause, pregnancy, and childbirth. However, men can also experience incontinence due to a variety of reasons, such as prostate gland problems.
You’ve Given Birth
Postpartum Stress incontinence (SUI) impacts around 33% of women after giving birth. Pregnancy and childbirth can impact the structure of your pelvic floor, so women who have given birth are at higher risk of having pelvic floor disorders.
Age
As you age, you lose muscle tone around your bladder and urethra. Age-related changes can reduce the amount of urine your bladder can hold and increase your chances of involuntarily releasing urine.
Being Overweight
Holding a significant amount of extra weight increases pressure on your bladder and surrounding muscles, weakening them and allowing urine to leak out when there is sudden pressure such as a cough or sneeze.
Family History
Certain people may be more genetically predisposed for urinary incontinence. If you have a close family member with urinary incontinence – particularly urge incontinence at a younger age – your likelihood of developing the condition is higher. However, this is only one factor, and just because you have a family member with the condition doesn’t mean you will necessarily have to deal with it.
How Incontinence Can Affect Your Life
Living with incontinence can take a heavy physical and emotional toll on the sufferer. It may require constant vigilance, and you may need to wear protective underwear or pads. You may be haunted by the ongoing worry of leakage, which can be exhausting. Moreover, incontinence may irritate your skin as it is constantly being exposed to moisture, resulting in infections or rashes and further discomfort if managed improperly.
Incontinence can also have a profound emotional impact. We’ve been bred from childhood to feel shame, embarrassment, and anxiety around incontinence, which can be compounded when it occurs in social settings. This can cause somebody to withdraw from social interaction and avoid spending time with loved ones due to fear of having an accident.
Addressing Urinary Incontinence
It’s important to address any concerns about UI, or if you think you have UI, with your health care provider. Often, they can help you prevent or control symptoms.
If your urinary incontinence isn’t severe, there are a number of steps your health care professional may recommend to try and control your symptoms. Lifestyle changes you can do on your own include:
- Timing the amount of liquid you drink
- Limited alcoholic, carbonated, and caffeinated beverages
- Remaining physically active
- Maintaining a healthy weight
- Avoiding constipation through diet and medication
- Not smoking
- Training your bladder through urinary scheduling or keeping a bladder diary
- Performing pelvic floor muscle exercises regularly
- Practicing methods to suppress your urge to urinate; this is called bladder training
Your health care professional may also prescribe additional steps to help you with your UI, including:
- Prescribing medications to help relax your bladder
- Using botox to help relax the bladder and lower the chances of leakage
- Utilizing medical devices such as a pessary or a catheter to help with incontinence
- Bulking agents may be injected near the urinary sphincter to bulk up the area around the urethra and help close the bladder opening to prevent leakage
- Electrical nerve stimulation
- Surgery


Discover how Laselle can help you prevent incontinence.